Updates & Press
Country Featured | October 14, 2020
The Escalating COVID-19 Crisis in Syria: Humanitar
Author | MedGlobalComms

The COVID-19 crisis in Syria is reaching a tipping point as hospitals become overwhelmed, testing remains limited, and cases are surging across the country. The impact of the pandemic is adding to an already dire humanitarian situation in Syria, nine years into an emergency conflict that has led to staggering levels of death and need inside the country, decimated the country’s infrastructure, and led to the world’s largest displacement crisis.
On October 1, MedGlobal hosted the webinar “The Escalating COVID-19 Crisis in Syria: Humanitarian and Health Update” focusing on the COVID-19 crisis throughout Syria, giving a picture of the crisis, response, and key needs in different governorates. Speakers gave insights into the COVID-19 response and updates from medics inside Syria. Below are the highlights from each panelist’s remarks.
Dr. Zaher Sahloul
President and Co-Founder of MedGlobal
“No one knows what the real COVID-19 numbers are, the official numbers are only the tip of the iceberg.”
“This is the only country where I’ve heard that patients need to purchase their own oxygen and ventilators to be treated at home because hospitals are not accommodating these patients. Because 8 out of 10 Syrians are below the poverty line and cannot afford this equipment, many people have died without being treated, they suffocated to death inside their homes.”
- At least 50% of healthcare providers have fled due to the targeting of hospitals and health workers. Health infrastructure has been destroyed, especially in the northwest, but even in government-controlled areas hospitals have been poorly managed and faced growing shortages of specialists.
- The Syrian government has only reported roughly 4,000 cases of COVID-19 and 200 deaths. However, physicians and experts in Syria believe that the actual number of cases is much higher. Some medical leaders in Syria have estimated that the actual number of COVID-19 cases may be over 110,000 in Damascus alone.
- Part of the problem is that testing in Syria remains extremely low. Only 35,000 tests have been conducted in government-held areas since the start of the pandemic. In comparison, Lebanon and Jordan are conducting 12,000 and 16,000 tests per day respectively and have much smaller populations than Syria.
- A dire lack of resources has also exacerbated the crisis. Personal protective equipment (PPE) is essential for the safety of both health workers and patients, but many physicians are now having to buy their own. This has contributed to an increase in infections among doctors and according to the Healthcare Union in Syria, at least 61 health workers have died from the virus. As a consequence, some doctors are reluctant to treat patients with COVID-19 and private hospitals closed their doors to protect their other patients.
- Each urban area has only 2 to 3 hospitals to treat COVID-19 patients. In Damascus, there were only 2 hospitals dedicated to treating COVID-19 patients, leading to long lines and people dying in crowded emergency rooms. For many Syrians, accessing treatment requires them to purchase their own oxygen concentrators and ventilators – an insurmountable barrier in a country where eight out of ten people live in poverty.
Dr. Naser Almhawish
Surveillance Coordinator for the Early Warning Alert and Response Network (EWARN) of the Assistance Coordination Unit
“To purchase a few thousand N95 masks… we had to wait more than one month.”
“The absence of good governance in the field is a huge issue because you do not have accountability.”
- The situation in northwest Syria has been developing rapidly in the last month.
- We can divide the COVID-19 response in the northwest into two stages: before the first cases were identified in July, and since COVID-19 cases have been confirmed. The closure of the borders around northwest Syria isolated the area and initially delayed the spread of COVID-19. Now, coordination and surveillance is essential for identifying gaps in the response and efficiently allocating resources.
- Expanding laboratory capacity for testing is critical, as is protecting health workers. Nearly 30% of confirmed cases are among health workers and the quarantining of staff for two weeks has devastating consequences for the health sector.
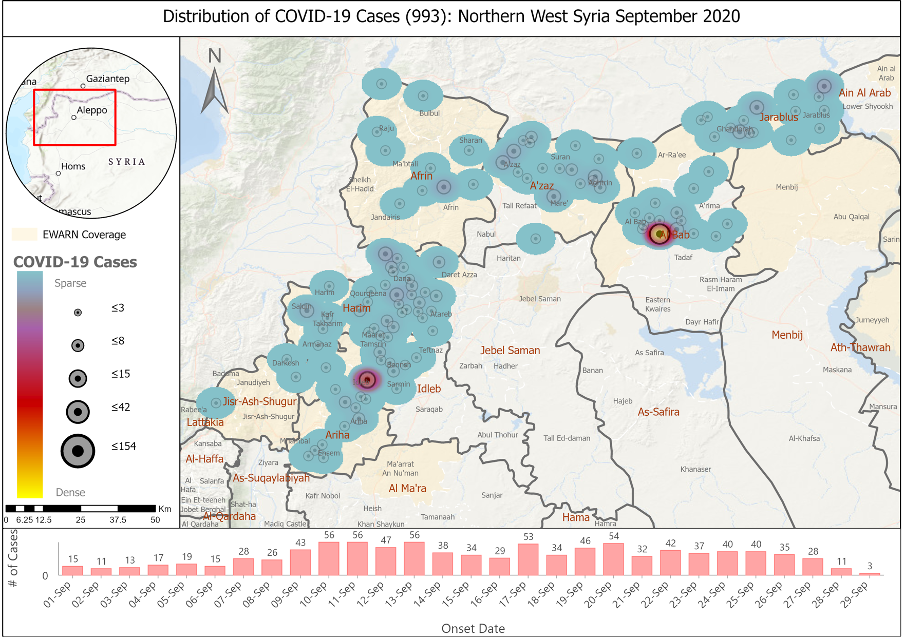
- Between July and August, there were only around 100 confirmed cases total in northwest Syria. In September, there have been 990 cases confirmed, and we know this is not all.
- Major challenges include the displacement of people, limited lab capacity, overwhelmed staff and shortages of healthcare providers, coordination issues and weak governance, and stigma which lead to people denying potential symptoms and prevents people from getting tested.
- The lack of PPE is greatly affecting healthcare providers. It’s also important to note that other safety and protection issues continue to affect healthcare providers, such as attacks on hospitals and airstrikes.
Hazem Rihawi
Senior Programs Manager of the American Relief Coalition for Syria (ARCS)
“This is the time now to increase the funding and the support for humanitarian responses coming into the northwest, the northeast, and government-controlled areas.”
“The health systems even in developed countries were struggling to be able to control this and you can imagine in a conflict zone like Syria it will be a further issue.”
- Research from the NWS Modelling Team at the Covid Modelling Consortium estimates that the COVID-19 peak will happen in mid-November if limited interventions happen.
- There are only 75 hospital beds in the northwest available for COVID-19 patients, which is much lower than needed. Hospitals in the northwest are already at 90% capacity.
- The time is now for countries like the United States and other stakeholders to increase humanitarian funding to all areas of Syria before the number of cases peaks in the coming weeks.
COVID-19 Response Coordinator
Northeast Syria Forum
“Social stigma continues to be a significant issue. People tell us that they don’t ring the hotline because they don’t want the neighbors to see an ambulance… they don’t want the rumor to get out that they might have the virus.”
“Just because we have beds which are currently operational does not mean that the quality of care is necessarily assured.”
“The impact of the UN Security Council Resolution 2533 renewal, or non-renewal you could say, is that to have a predictable supply line in northeast Syria, we do require multiple modalities, whether that is UN cross border shipments under a Security Council resolution, NGO local procurement, NGO cross border procurement, or cross-line assistance from Damascus. We need this because we know that any one of these pipelines can break down.”
- As of September 30, there have been 1,670 confirmed cases of COVID-19 in northeast Syria, including 67 deaths and 437 recoveries. At least 200 health workers are in self-isolation or quarantine and 10 health facilities have closed either a section or entirely. There is a gap of 818 hospital beds and 236 intensive care unit beds and virtually all patients who have been ventilated have died. Despite the crisis, which is on track to worsen significantly, there are no movement restrictions or lockdowns in place and there is minimal adherence to personal preventative measures.
- One of the key challenges that needs to be addressed in the northeast is the low levels of risk perception among the population. It is important to remember that over the last nine years, the people living in this part of Syria have experienced immense hardship from the Syrian conflict, living under ISIS, and dealing with an economic crisis. Civil leaders have downplayed the danger of the virus and stigmas around COVID-19 keep people from reporting symptoms and seeking treatment. There are low levels of hospitalization as people are dying in their homes rather than seeking medical care and those that do often wait until they are at advanced stages of the virus.
- The closure of the Al Yarubiyeh border crossing into northeast Syria has further intensified the crisis by disrupting supply chains. PPE in hospitals is being washed and reused and some health facilities have instituted policies against using PPE unless the patient is confirmed to have COVID-19. Supplies for conducting testing are also in great demand and there is concern that testing capacity will fall to zero by the end of the year.
- Key needs for managing the COVD-19 crisis include high levels of funding through 2022 and improved coordination between health facilities and different levels of governance.


